2023 was a difficult year for us. It was a year that made me suddenly feel very old and fragile. I’m still coming to terms with a lot of what happened.
Irene was diagnosed with cancer in February of 2023. Our life has changed, and we are still figuring out what it all means.
The diagnosis- a timeline
Irene had some severe shoulder and arm pain in February. It got bad enough that we went to the local emergency on February 27th. During that visit X-rays and other diagnostics were performed, and the initial diagnosis was some kind of tendonitis in the shoulder.
Irene mentioned somewhat offhandedly during the exam that she had noticed a lump in her left breast. The examining Doctor’s demeanour changed as he examined her based on this new concern. He ordered a series of additional tests including a mammogram and ultrasound. He also booked Irene in for some physio for her shoulder pain. Neither Irene nor I had been able to get a family doctor by this time, but the examining Doctor immediately added Irene to his patient list.
The initial tests had been completed by March 2nd, and the initial indicators were that the lump might be cancer. By March 12th we returned to emergency with more severe shoulder pain. Irene was unable to sleep soundly because the pain was so bad, and she was despondent. The physio wasn’t helping, and the therapist notified the Doctor about Irene’s severe pain and tears. The Doctor ordered a biopsy and CT scan.
The breast cancer diagnosis was confirmed on March 14th via the biopsy. The CT scan suggested some oddities in Irene’s vertebrae. A bone scan as well as X-rays with contrast were ordered and completed by April 4th. CT scans with contrast were completed by April 6.
On April 17th we had our first zoom call with what was to become Irene’s lead oncologist: Dr. Sara Taylor. Her diagnosis was stage 4 metastatic breast cancer; grade 3, with lesions in lymph nodes and ‘highly probable’ lesions in the C4/C5/C6/C7 vertebrae. I recall that this was the first time we heard the words ‘incurable’, but I could be mis-remembering. The tumour was identified as HER2 positive (reactive), which identifies the specific types of treatments it should respond to.
A treatment team was assembled with plans for starting chemo ‘immediately’ along with a radical mastectomy later in the year. Irene met with the surgeon who recommended completing a course of chemo to reduce the breast tumour size before surgery.
On April 18, Irene had a severe nose bleed that led to hospitalization and ‘packing’ of the sinuses. On April 20th she had another CT scan, looking in more detail at the spinal lesions and checking (I believe) for any condition that might cause the nose bleeds.
Also on April 20th we had our first ‘pre-chemo’ meeting with the chemo treatment specialist doctor in Trail: Dr. Kowaluk. By this point it became clear to me at least that we had a full medical team caring for Irene who were all working together and sharing details in near real-time. Irene’s treatment was pushed to the ‘top of the list’. We met Irene’s chemo treatment coordinating nurse, saw the oncology infusion clinic, and started to understand what was ahead of us. Irene had been booked in to the Kelowna cancer clinic for priority targeted radiation treatment regarding the cervical spine lesions.
This was followed by additional diagnostics. An echocardiogram on April 22, and an MRI on April 24. Irene received an emergency call the day after the MRI telling her to immediately wear a neck brace and get an Aspen collar fitted as quickly as possible.
The Aspen collar came along with strict rules for movement, including restrictions on driving and a complete ban on horseback riding. When asked how long she’d have to wear the collar she was told ‘indefinitely’, 24 hours a day, 7 days a week.
All of the medical professionals we dealt with during this process were extremely considerate and kind. I sincerely cannot say this enough, or thank them adequately. Irene’s phobia of needles was a continual challenge, but every possible accommodation was made so that the treatments could be tolerated by her. I was and still am amazed.
The treatment
We started on Irene’s chemo treatments on April 26. The first eight rounds were scheduled for three drugs each treatment with three week ‘breaks’ between rounds.
The treatment protocol itself consisted of three drugs administered (infused) over a period of about eight hours: a protocol abbreviated as BRAVPTRAT or “BReast AdVanced Pertuzumab TRAstuzumab Taxol (Paclitaxel)”.
Of these the ‘nastiest’ was the Paclitaxel. This is the kind of drug where the nursing staff wears full ‘bunny suits’ just to handle the IV bags: a drug that must be proceeded by other drugs to prevent severe reactions, and which renders the patient temporarily ‘toxic’ i.e.: everything coming out of her body is dangerous. It also destroys the immune system and causes the patient’s hair to fall out: the kind of drug most people think of when imagining cancer treatment.
The first chemo treatment went well. Irene had mild reactions to the chemo, a result that thankfully continued throughout the first eight rounds. She was tired and a bit ‘off’ for a few days after each round, but generally tolerated the worst drugs extremely well.
On May 1st Irene had surgery to install a ‘port’ (portacath). The main purpose of this was to make the chemo infusions easier with fewer needle-related challenges. On May 3rd we went to Kelowna for five days of radiation treatment for Irene’s vertebrae. The process was amazingly ‘easy’, fast, and essentially painless. We met with the specialist Doctor first who explained the details. They then fitted her with a ‘mask’ so that she could remain still during the treatment and the precise laser-aligned targets identified by the Doctor could be repeatedly treated.
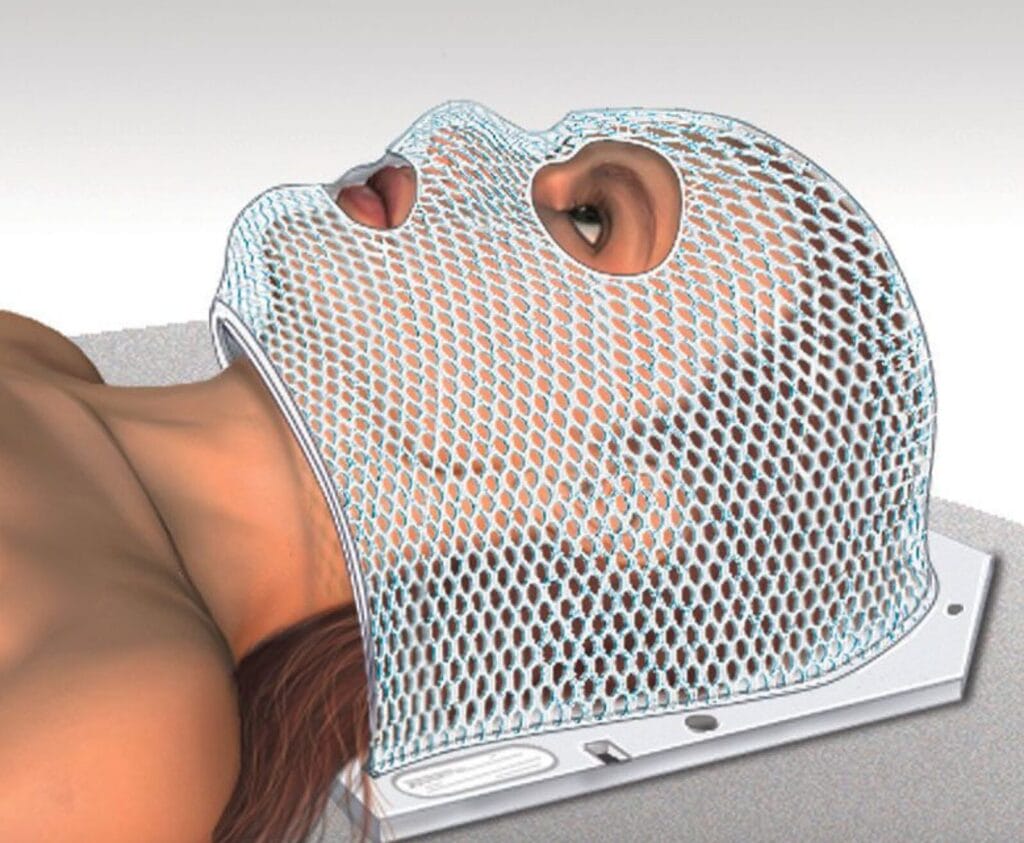
An example of what the radiation mask looks like
Each actual radiation treatment took about 30 minutes, and there were five such treatments in the recommended plan.
Interestingly, Irene was able to pretty much completely stop the course of powerful pain killers she had been on for her shoulder pain within a few days of the radiation treatment. I suspect that the tissue around the vertebrae was inflamed and pressing on the nerves for her arms. In my theory, the treatment reduced the inflammation and eliminated the pressure on the related nerves, resolving the pain.
Irene began regularly ‘begging’ to be able to stop wearing the Aspen collar. All the doctors basically said ‘no’: the vertebrae had been damaged by the cancer lesions and the risk of catastrophic fracture was too great. But this remained an ongoing challenge: the collar directly reduced Irene’s ‘quality of life’ to the point that it caused some intense and distressing discussions.
We made it through all eight rounds of the first ‘course’ of treatment without serious incident. Irene continued to have mild reactions, there were no more nose bleeds, and there was no recurrence of the severe neck and shoulder pain. The three-drug protocol meant a full eight hour day for each round, and if anything went wrong that could mean a ten-plus hour day. We had a couple of those: once one of the drug bags leaked which resulted in a ‘full toxic waste’ cleanup response and then replacement of the drug which added a couple of hours easily.
I kept thinking: this is the same stuff that they are putting into Irene’s body, and it takes a team of four in full hazmat gear to clean up a teaspoon of it that spilled on the floor.
The current situation
After the first eight rounds, Irene’s treatment switched to a two drug protocol with just the monoclonal antibodies: Pertuzumab and Trastuzumab. This is much better: maybe four hours per round and, without the nasty Paclitaxel, is much easier on Irene’s body. And her hair is starting to come back, which makes her happy. We’ll be on this protocol now indefinitely: until it stops working.
Irene has had a number of diagnostics to review the progress of the treatment. Putting the various pieces together: the lesions on the vertebrae are completely ‘gone’, and there are indicators that the bone has been healing. The cancer in the lymph nodes is likewise essentially ‘gone’, but has left behind damage that means that Irene is suffering from some edema in her left arm. The tumour in the breast has shrunk and become less ‘cohesive’, so it is almost intangible now.
One point of confusion arose: the ‘incurable’ nature of the cancer led the medical team in May to cancel plans for a mastectomy surgery. This cancellation was never made clear to us, and we were confused when we found out in August that the surgery was no longer happening in the fall. Apparently this is not a ‘bad’ thing: it didn’t mean that the prognosis was ‘worse’, just that the balance of risks meant that the surgery was no longer as helpful as simply continuing the chemical cancer treatments.
In August Irene received permission to stop wearing her Aspen collar. The doctors have made it clear that she is still ‘at risk’ of vertebral fracture, but Irene is ‘allowed’ to manage that risk with some more flexibility. She has hope that she will be able to (carefully!) ride her beloved horse, Spirit, starting in the spring.
Every indicator is that the treatments have worked well and Irene has handled them without any serious side-effects. Irene is incredibly strong, both physically and emotionally. She’s had her bad days, of course, but the lady I love has been far more resilient than I could imagine myself being.
The future
The Doctors can’t make guarantees. Irene’s cancer is incurable, which means she’ll be getting some kind of treatment so long as it continues to be helpful for the rest of her life. But we had a good conversation with the lead oncologist, Dr. Taylor, on January 8th. We asked the ‘tough’ questions: various forms of “how long do we have?”
With no promises, the indicators are that every aspect of the treatment and Irene’s response has been near the top of expected outcomes. We should have years together. And if the current treatments stop being effective there are a whole new series of options for HER2 positive tumours that can be tried. So maybe more than just ‘years’.
Irene’s medical team has been extraordinary. The Trail hospital oncology clinic has been unendingly kind and supportive. The BC Cancer Clinic radiology team in Kelowna was likewise supremely patient and generous with their time. The lead oncologist, Dr. Taylor, was very informative, kind and helpful once we successfully connected up with her.
Despite all this good news, I really do feel like life is distinctly unfair. Irene and I were supposed to have a ‘golden years’ span of decades. There were plans that we had. Now… it isn’t so clear. I have to imagine a likely time in the future when I’ll be alone. I don’t like that future.
I’m retiring in 2024. My management team at work has been very supportive during 2023, granting me pretty much whatever time I need to support Irene. But I still feel ‘torn’ when work priorities conflict with what Irene asks. Retiring means I can eliminate a source of stress and be more available for whatever Irene wants: not just for her treatment, but for spending quality time together.
I’ve included a lot of detail here- probably more than any rational person would want to consume. I’ve found it somewhat cathartic: thinking through the sequence of the year has been good for me. But that isn’t necessarily a good reason for this post.
What I really imagine is that maybe someone else will find this detail ‘helpful’. Maybe they will be facing similar challenges and will find this post “cathartic” as well. Perhaps this imaginary person will see that, even with incurable cancer diagnoses, treatment can still grant hope.


Thank you sharing this Kelly. While I see and hear the pain associated with this past year, I also see joy in the love that exists between you and Irene. I cherish you both.
Thank you, Sharon, for commenting. It has been tough, but lots of people go through this kind of thing and worse.
What really has been surprising and so very helpful is how kind and supportive people have been. The wigs and such you shared, for example, were the start of Irene accepting her hair loss- and finding a new way to express herself.
Things aren’t ever going to be quite the same again, but they are getting better. The Aspen collar is collecting dust now, and Irene’s hair is starting to come back: peach fuzz for now, but soon she’ll need to start brushing it! 🙂
Thank you Kelly for the details
I am one of those people that likes to understand fully what is happening
and you have explained it very well
Corinne
Thanks for the comment, Corinne!
I am glad you get something out of the detail. I knew it was ‘too much’ as I was writing it, but it was kind of therapeutic for me to document the sequence and capture the facts.
As I said in the original post: I would like to imagine someone else facing a similar diagnoses can get some comfort from the documentation of what Irene and I experienced. My little ‘corner of the internet’ doesn’t draw much traffic, but it is a nice thing to imagine at least.
Kelly, thank you for sharing and explaining so well what you two have been going through. We are glad things are improving. You and Irene have incredible strength and courage. Stay strong!
Thank you for your comment!
We hope your 2024 is a good one. From our side, we are looking forward to fewer ‘life changing’ surprises and a start to enjoying our retirement together.
Pingback: Retirement: Looking back at the work | Kelly's World- A View into the mind of Uber Geek, Kelly Adams
Pingback: Road trip 2023: A Motorcycle Journey through Illness – Geek on a Harley
Pingback: Who is Kelly Adams? | Kelly's World- A View into the mind of Uber Geek, Kelly Adams
Thank you so much Kelly for sharing this. I hope Irene is feeling better now. Felt really happy to read how you supported Irene at each step during that difficult journey. I am 37 years old and on 2 Jan 2025 have been diagnosed with same stage 4 metastatic breast cancer grade 3 and I have been advised samr treatment plan by my oncologist. Your details has really helped me in understanding. I am just done with first chemo round and hope to get through remaining 7 rounds with strength. And after that i will also be on trastuzumab and pertuzumab for indefinite period. Enjoy your retirement with Irene.
Thank you for your comment, Neha. Best of luck in your treatments: everyone reacts differently, so be kind to yourself. The medications are amazing: not perfect, of course, but they can grant a good long life with plenty of opportunity for joy when they do their job.